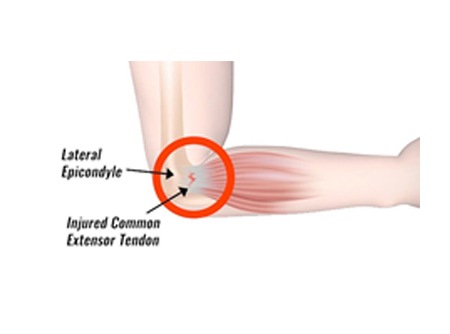
TENNIS ELBOW (LATERAL EPICONDYLITIS-LE)
- Approximately 40% of people will experience LE at some point in their life, prevalence being 1-3% within general population and 4-7 per 1000 patients visiting general medical practitioners.
- Approximately 50% of all tennis player experience some type of elbow pain, with 75-80% of these elbow complaints due to LE.
- It most commonly presents in men and women aged between 35-54 years.
- Increased BMI, high perceived exertion with repeated elbow and wrist flexion/extension movements being the risk factors for LE.
- Patients with rotator cuff pathology, De Quervain’s disease, carpal tunnel syndrome, oral corticosteroid therapy, and previous smoking history are also at risk of developing LE[3].
INCIDENCE
- LE is the most common overuse syndrome in the elbow. It is an injury involving the extensor muscles of the forearm. These muscles originate on the lateral epicondyle region of the distal humerus i.e outer part of the elbow. In a lot of cases, the insertion of the extensor carpi radialis brevis is involved.
- Patients generally complaint of pain in the outer part of the elbow and forearm with difficulty in gripping activities, wrist movements and extension of second or third fingers. Pain may have an insidious onset with no specific causal activity. Swelling may/may not be present.
- Exploratory research indicates that neck pain is more common in people with LE.
- Investigations such as Ultrasound and MRI have high sensitivity but low specificity in detecting tennis elbow because, structural abnormalities identified on imaging tend to be consistent across all tendinopathies.
ABOUT THE CONDITION
- Exercise for core strengthening of the muscles may be more effective at reducing pain and improving function than other interventions such as US, placebo US, and friction massage, but there may be no difference in effect between different types of exercises.
- manual therapy techniques to the elbow, wrist and cervicothoracic spine may reduce pain and increase pain-free grip strength immediately following treatment there was conflicting evidence for the effectiveness of orthoses in providing pain relief or improvement in function compared with placebo or no treatment. Elbow orthoses may be as effective as corticosteroid injection in the short term; however, there was only one study to support this claim. There was no compelling evidence that any one orthosis is superior to another in the short term, or that adding an orthosis to another treatment provides any additional benefit.
TREATMENT
- Dry needling/soft tissue release for the flexor compartment to ease the effort of extension.
- Strengthening of the shoulder girdle and posture correction thereby improving proximal control and reducing the distal load.
- Taping techniques may help to offload the affected area.
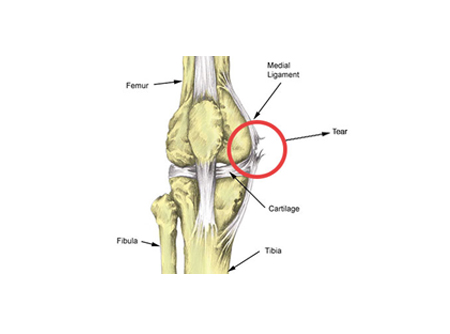
MCL STRAIN
- Medial collateral ligament (MCL) injuries of the knee are very common sports-related injuries and commonly occur in all age groups.
INCIDENCE
- MCL is present at medial side of the knee joint. It is a primary static stabiliser of the knee and assists in passively stabilizing the joint, provides the primary restraint to valgus loads at all degrees of flexion. It is also an important restraint to anterior tibial translation when the anterior cruciate ligament is injured.
- MCL has its superficial and deep layers.
- Patients complain of pain on medial aspect of knee with localized soft tissue swelling or echymosis.
- Patients may notice an audible snap or tearing sound at the time of injury. In minor cases of a MCL strain that is grade 1 , patients may be able to continue activity only to experience an increase in pain, swelling and stiffness in the knee after activity.
- In grade 2 or grade 3 injuries generally patient can’t continue the activity or is unable to weight bear due to pain.
- X-ray is performed to rule out any fracture or bony chip, Ligament Stress test helps the doctor determine the extent of injury and an MRI may confirm the diagnosis.
ABOUT THE CONDITION
- The majority of patients who sustain MCL injuries of varying severity can achieve pre-injury activity level with non operative treatment alone. Surgical reconstruction is indicated for isolated symptomatic chronic MCL laxity or combined ACL and MCL injuries or complete tibial avulsion tears.
- Grade 1 (25% fibers torn or over stretched) and Grade 2 (25 to 50% fibers torn) MCL injuries recover to preinjury status in 3 to 4 months with conservative management.
- Rehabilitation includes protected range of motion and strength training which gives excellent results and return to activity.
- Grade 3 requires surgical reconstruction of the ligament followed by 6 to 9 months of rehabilitation.
- POSTOPERATIVE CARE -The patient is kept non-weight bearing for three weeks in a long-hinged knee brace allowing 30-90 degrees of motion. At 3 weeks the patient is allowed to do full range of motion and weight bearing as tolerated. Progressive activities are started at about six weeks and the brace is gradually weaned off followed by strengthening and specific sports injury rehabilitation program.
TREATMENT
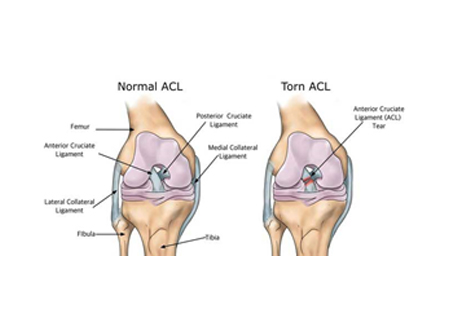
ACL INJURY
-
Anterior cruciate ligament (ACL) injuries are common, especially in young individuals who participate in sports activities associated with pivoting, decelerating and jumping (e.g. football, basketball, handball, gymnastics, downhill skiing).
Direct Contact: 30% of the cases, Non-Contact: 70% of the cases -
ABOUT THE CONDITION
The ACL is composed of densely organized, fibrous collagenous connective tissue that attaches the femur to the tibia. - The ACL is the primary (85%) restraint to limit anterior translation of the tibia. The greatest restraint is in full extension. It also serves as a secondary restraint to tibial rotation and varus/ valgus angulation at full extension.
- Symptoms of an acute ACL injury may include the following
- Feeling or hearing a “pop” sound in the knee,
- Pain and inability to continue activity,
- Swelling and instability of the knee,
- Episodes of "giving way" especially on pivoting or twisting motions,
- Restricted movement,
- Especially an inability to fully extend, tenderness around the joint.
- Diagnostic procedures like radiographs (x-ray) will reveal if any fractures associated with ACL injury. MRI will help us in determining the site and extent of injury.
INCIDENCE-
- Over 50% of all ACL Ruptures have associated Meniscal injuries. If seen in combination with a Medial Meniscus Tear and MCL Injury, it is called O’Donohue’s Unhappy Triad which has 3 components: Anterior Cruciate Ligament (ACL) Tear, Medial Collateral Ligament (MCL) Tear, Meniscal Tear, it is resultant of a valgus stress to the knee.
ASSOCIATED INJURY:
- Immobilization period of 3-4 weeks with rest and icing.
- If patient needs a surgical intervention then pre surgery 4-8 weeks of prehabilitation program and post-surgery 4-6months of rehabilitation is needed.
- Exercises to strengthen affected as well as contralateral limb.
- Gait correction and training.
- Balance and proprioception exercises
- Sports physiotherapy treatment.
TREATMENT
REFERENCES
http://emedicine.medscape.com/article/89442
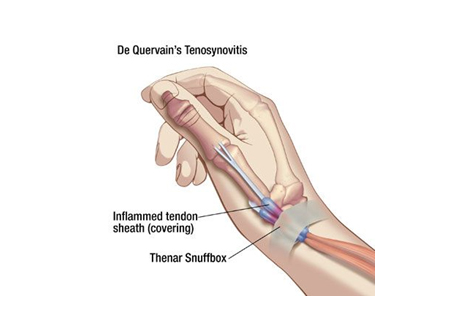
DEQUERVAINS TENOSYNOVITIS
- It is second most common entrapment tendinitis of the hand and wrist with prevalence being 8-17%.
- It is 10 times more frequent to be found in women heath symptoms as compared to men. The condition is most common between 30-50 years of age.
INCIDENCE
- De Quervain tenosynovitis is an entrapment tendinitis of the tendons contained within the first dorsal compartment at the wrist.
- The tendons of the abductor pollicis longus and the extensor pollicis brevis are tightly secured against the radial styloid by the overlying extensor retinaculum. Any thickening of the tendons from acute or repetitive trauma restrains gliding of the tendons through the sheath.
- Movements at the thumb, especially when combined with radial or ulnar deviation of the wrist, cause pain and perpetuate the inflammation and swelling, tender to touch.
- Causes may include chronic overuse injury, direct trauma leading to scar tissue formation, or inflammatory arthritis.
ABOUT THE CONDITION
- Thumb spica brace (if needed) reduces pain by immobilizing the thumb and the wrist joint, thereby preventing thumb metacarpo-phalangeal joint flexion and wrist ulnar deviation.
- Icing to reduce swelling and tenderness
- Ultrasound therapy
- Soft tissue releases for the forearm muscles to relax them and enhance drainage of fluid from the muscle tissue.
- Along with increasing control of the wrist muscles, eccentric exercises will also assist soft tissue mobilization and promote healing.
- Daily activity modifications are required on a long term basis to allow for neutral wrist positioning.
- Sometimes corticosteroid injection is delivered into the first dorsal compartment if the pain is severe.
- Surgical release of first dorsal compartment needs to be performed if the pain doesn’t subside with conservative management.
- Postoperative physiotherapy is started 2 weeks post-surgery which includes improving range of motion, scar and edema management.
- Strengthening and return to functional activity is gradually started after 4 weeks of surgery.
TREATMENT
References-
https://www.physio-pedia.com/De_Quervain%27s_Tenosynovitis
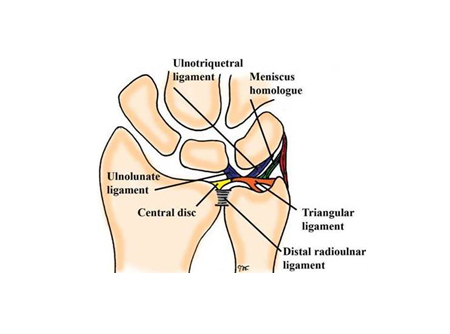
TFCC INJURY
- Commonly associated with sports which involve weight bearing through wrist (gymnastics) or involving repetitive radial and ulnar deviation of the wrist (javelin throwers, discus throwers).
- Attritional tears or degenerative pathology involving the TFCC are common, with a reported incidence of tears being greater than 50% of those over the age of 60 years.
- It is estimated that TFCC injury occurs in up to 80% of displaced distal radius fractures.
INCIDENCE
- Triangular fibrocartilage complex suspends distal radius and ulnar carpus from distal ulna. It is the major ligamentous stabilizer of the distal radioulnar joint (DRUJ) and the ulnar carpus.
- Causative factors for TFCC injuries are
ABOUT THE CONDITION
- Ulnar deviation with load compression on TFCC (fall on an outstretched hand)
- Forced ulnar deviation (swinging a racket or bat)
- Commonly associated with positive ulnar variance (this is when the joint surface of ulna at the wrist joint is more longer than the joint surface of radius) which occurs mostly post-surgery or post fracture.
- Patients mostly presents with:
- ulnar-side wrist pain
- frequently accompanied by clicking
- weakness in grip and instability
- X-rays may reveal any avulsion fractures associated with injury and MRI is highly recommended with high sensitivity and specificity for identification of tear.
- Initial treatment consists of rest and icing.
- Conservative treatment for 6 months is advisable if there is no instability.
- Dry needling the TFCC helps to reduce pain.
- Gradually proceeding to muscle activation and strengthening followed by stability and proprioceptive exercises in order to regain functional activities.
- If congenital ulnar variance is present, conservative management is started after 18years of age (i.e. post complete bone maturation) which includes improving stability in the wrist joint.
- Strengthening the shoulder girdle will help to off load the load on the wrist
- If conservative management fails, surgery is considered.
- Depending on the cause of injury the type of surgery will vary which includes arthroscopic repair, arthroscopic debridement, ulnar shortening, and the Wafer procedure.
- Corticosteroid injections are also preferred in some cases.
- Length of physiotherapy varies from 4 to 16 weeks depending on surgeon’s preference.
- Activity modifications are required on a long term basis.
TREATMENT
REFERENCES
https://www.ncbi.nlm.nih.gov/books/NBK537055/
https://www.physio-pedia.com/Triangular_Fibrocartilage_Complex_Injuries#cite_note-14
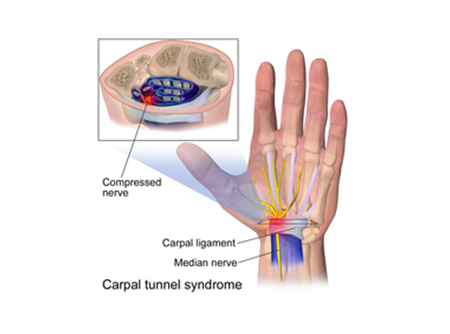
- CARPAL TUNNEL SYNDROME
- The estimated prevalence of CTS is 4-5% of the population.
- CTS usually affect people between 40 and 60 years.
INCIDENCE
- Carpal tunnel syndrome (CTS) is a condition in the wrist. It is caused by compression, traction, pinching, squeezing or irritation of the median nerve, while it runs through the transverse carpal ligament.
- The median nerve runs from the forearm to the palm side of the hand. It controls sensations to the palm side of the thumb and fingers, except for the little finger. It also allows the fingers and thumb to move.
- The CT is very rigid and narrow, so a little swelling of the tendons causes a lot of compression on the median nerve.
- The carpal tunnel syndrome generally starts with tingling or numbness in the thumb, the index finger, the middle finger and the lateral half of the ring finger. This sensation often appears while holding an object like a phone or steering wheel.
- Symptoms develop gradually, as the disorder progresses, the feeling of tingling or numbness may become constant and patients may complain of burning pain. The final symptoms are weakness and atrophy of the muscles at the base of the thumb.
- Probable risk factors for CTS include age, gender, diabetes , hypothyroidism , obesity , family history of CTS , menopause and concurrent pathologies such as rheumatoid arthritis. Also tobacco consumption and smoking can be risk factors.
- Diagnostic procedure like EMG/NCV studies can determine if there is any muscle damage and can rule out other conditions.
ABOUT THE CONDITION
- Splint and activity modifications
- Soft tissue release or dry needling of the muscles along the course of the nerve to relieve the compression on the nerve is done.
- Neck joint mobilization to reduce neck stiffness which will help to free the nerve root.
- Median nerve gliding exercises are required to mobilize the nerve.
- Rigid taping for the wrist for relief in acute stage.
- Strengthening of scapular and wrist muscles to reduce the load on the muscles entrapping the nerve.
TREATMENT
REFERENCES
https://www.physio-pedia.com/Carpal_Tunnel_Syndrome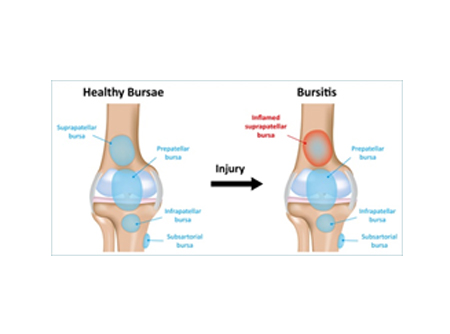
- BURSITIS
- Bursitis accounts for 0.4% in general population.
- The incidence of bursitis is higher in athletes, maximum being 10% in runners.
INCIDENCE
- Bursitis is the inflammation of a bursa.
- Bursae are saclike structures between skin and bone or between tendons, ligaments, and bone. They are filled with thin layers of synovial fluid. They produce fluid that lubricates and reduces friction between the structures that they are interposed in.
- When a Bursa gets inflamed due to altered biomechanics , it swells, develops friction and starts irritating the muscle tendon it is supposed to protect. This leads to a continuum of irritation of the tendon and bursa leading to a cycle of pain, spasm and associated tendinopathy.
- Symptoms of bursitis may include localized tenderness, pain (aggravated by movement of the specific joint, tendon, or both), edema, erythema and restricted Range of Movement. They may have a history of repetitive movements, trauma or inflammatory disease.
ABOUT THE CONDITION
- Subacromial bursa , olecranon bursa, trochanteric bursa, prepatellar and infrapatellar bursa are the most commonly affected bursae.
- Bursitis may occur due to constant friction or pressure, by an overuse injury or trauma, erratic loading or sepsis (infection after traumatic injury).It may also be associated with an underlying systemic condition.
- Rest and icing to reduce bursal pain and inflammation.
- Taping to offload the bursa.
- Strengthening and stretching exercises to correct the altered biomechanics around the joint in order to correct the movement pattern and reduce the pressure/irritation on the bursa.
TREATMENT
REFERENCES
http://emedicine.medscape.com/article/2145588
ERGONOMICS RELATED PROBLEMS
Ergonomics is the study of efficiency of people in their working environment. The tools and machines used in the workplace should be designed according to the physical demands of the people working there. Thus Ergonomics aims to improve workspaces and environments to minimise the risk of injury in the workers.
Muscles, tendons, joints and nerves are susceptible to injury when stressed or traumatised repeatedly, or over an extended period of time. Regardless of the nature of the work, a large proportion of the working population’s time is spent engaged in repetitive movements and maintaining postures for extended periods of time. The reported incidence of work-related back and neck pain, and carpal tunnel syndrome, is between 15-60%, indicating that a high proportion of the working population is at risk of developing one or more work-related musculoskeletal disorders. The parts of the body that are most commonly affected are the lower back, neck and shoulder girdle, and upper limbs.
We perform a detailed ergonomic assessment of your work place, evaluate your posture when at work, assess your strengths required to perform your job/task, co-relate it with your pain and plan a rehabilitation programme which includes posture correction exercises that will allow you to do your job pain free and with a better efficiency thus giving better results.
PLANTAR FASCIA SYNDROME (PLANTAR FASCITIS)
-
1-4% in general population
10% in the running population
INCIDENCE
ABOUT THE CONDITION
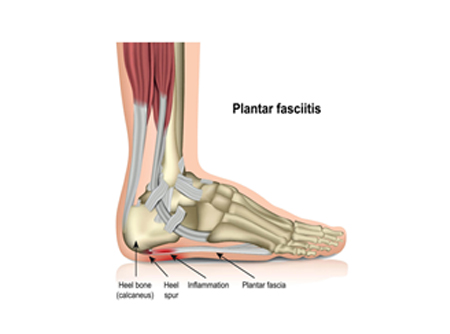
Plantar fascia is a thick band of tissue that runs across the bottom of your foot and connects your heel bone to your toes. Earlier the condition was coined as plantar fasciitis because it was believed that there is inflammation predominantly in plantar fascia. Since the recent evidence suggests that the inflammation and degeneration of the plantar fascia and the structures surrounding it occur simultaneously, the term plantar fasciopathy was coined.
The probable causes of the same can be abnormal pressure on the foot due to erratic loading, tightness of structures surrounding the foot, especially calf or altered biomechanics of the lower limb or the entire kinetic chain leading to increased pressure on the foot and ankle.
- Icing
- Activity modifications
- Taping to offload the pressure on plantar fascia
- Dry needling/release for tight muscles.
- Core Strengthening for hip,core and foot intrinsics.
- Neural mobilisation may be required in case of any nerve affection.
TREATMENT
.jpg)
MEDIAL TIBIAL STRESS SYNDROME(MTSS)
INCIDENCE
4-35% in runners and military population.
ABOUT THE CONDITION
Shin splints is the commonest term used for MTSS, the pain along the inner side of lower 2/3rd of the leg.
Causes can be high impact or repetitive loading activities like jumping or running.
It is a syndrome which includes multiple causative factors like weak or tight hip and calf muscles, tight lumbar paraspinals, weak lower abdominals and hip flexors. All these changes leads to altered biomechanics loading the bone there by leading to a stress reaction leading to stress fracture.
The main symptom is dull pain at distal 2/3rd of the leg. It is generally activity dependent. Pain on palpation is typically present following activity for few days.
The most common complication following MTSS is stress fracture of tibia due to continuous micro trauma on bone caused by loading activities.
MRI or Ultrasonography can be used to rule out stress fracture.
- Load management is the key in resolving this syndrome
- To reduce high impact activity and to continue low impact activity and strengthening of kinetic chain.
- Icing
- Dynamic or kinesio taping to offload tibialis posterior muscle.
- Release / dry needling for tight and fatigue calf and hip muscles.
- Strengthening of lower abdominals, hip flexor and extensor muscles.
- Proprioceptive and balance training.
- Functional fitness training regime needs to be followed to prevent re-injury
TREATMENT
LUMBAR CANAL STENOSIS
INCIDENCE
The prevalence of lumbar canal stenosis has been suggested as ranging from 1.7 to 13.1%. The prevalence of acquired LSS increases with age with women getting affected more than men.
ABOUT THE CONDITION
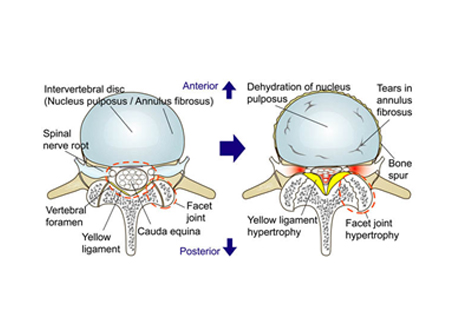
Lumbar spinal stenosis is the narrowing of the spinal canal and compression of spinal cord and its nerves producing symptoms like pain , tingling numbness and weakness.
The most common cause of it being degeneration, it can also be caused due to other reasons including congenital, post-traumatic, spondylolisthetic, tumour-compressing.
Symptoms initially start with bouts of Low back and radiating pain. The classical complaint in lumbar stenosis is neurogenic (or spinal) claudication. These symptoms include radiating pain, tingling and weakness of leg. Usually has bilateral leg complaints and distribution of pain is dependent on the area of stenosis(compression). Additional symptoms in the legs may be fatigue, heaviness, leg cramps, as well as bladder issues.
Prolonged standing and walking , back bending becomes difficult or aggravate the symptoms. Forward bending, sitting, stooping or lying helps relieve the symptoms.
At Replay Physio physiotherapy and rehabilitation center, we assist you in avoiding the pain of the injury and help you get fitter faster.
- Medical management includes NSAIDS, pain-relievers, muscle relaxants, oral opiods on a short term basis and B12 and tricyclic antidepressants to reduce nerve pain.
- Decompressive Surgery for spinal stenosis is indicated for significant myelopathy,radiculopathy, and/or neurogenic claudication.
TREATMENT
- Spinal Mobilization to improve mobility of vertebral joints and nerve in the available space of the lumbar canal.
- Releasing tight paraspinal muscles either manually or by dry needling.
- Neural mobilisation to mobilise the nerve and relieve the neural symptoms.
- Spinal mobility exercises to maintain the mobility of the lumbar spine.
Physical therapy would include:
.jpg)
PROLAPSED INTER-VERTEBRAL DISC(PIVD)
INCIDENCE
1% to 3% with the highest prevalence among people aged 30 to 50 years, with a male to female ratio of 2:1.In individuals aged 25 to 55 years, about 95% of herniated discs occur at the lower lumbar spine (L4/5 and L5/S1 level); disc herniation above this level is more common in people aged over 55 years.
ABOUT THE CONDITION
PIVD is a condition in which disc between the two vertebrae bulges/protrudes out leading to compression of spinal cord or nerve.
The human spine is made up of alternating vertebrae and intervertebral discs extending from the neck to the tail bone. The intervertebral discs are the ‘shock absorbers’ of the body and are composed of an outer strong fibrous membrane and an inner ‘jelly-like’ nucleus giving both strength and elasticity. A disc prolapse occurs when there is weakening in the outer membrane which leads to a protrusion of the inner nucleus. This protrusion usually heads towards the spinal canal thus compressing them giving rise to the symptoms.
Disc herniation can occur in any disc of the spine, but the two most common site are lumbar disc herniation and cervical disc herniation
As we grow older, our intervertebral discs begin to lose water content. However, several other factors may encourage or exacerbate prolapsed discs in both the young and the elderly, such as:
- Repeated improper movements that place stress upon the spine, often due to sports, improper lifting and even sitting or sustained postures for prolonged period of time.
- Sudden injuries or traumas that might occur during a high-impact sport, fall or car accident
- Sedentary lifestyle
Symptoms include mild to severe back pain which can be caused by muscle spasm and may radiate to leg due to nerve irritation. In case of cervical disc herniation in can radiate to the hand. There may be pins like sensations, tingling, numbness, burning , pully like sensation and weakness in the affected area. In severe cases there may be bladder and bowel incontinence and weakness/paralysis of the muscle supplied by that particular nerve root.
Physical assessment along with an MRI scan can confirm the diagnosis.
TREATMENT
Medical treatment would include muscle relaxants, anti-inflammatory , analgesics(pain-killers), tricyclics for nerve pain.
- In acute state complete rest with medications for 3-5 days.
- Bracing with lumbar corset or rigid tape to support weak or tight muscles which are in spasm.
- Dry needling of the tight paraspinals or surrounding muscles.
- Joint mobilisation to improve thoracolumbar junction there by relieving the overload off the lumbar spine.
- Lumbar core muscles activation which includes transverses abdominis , pelvic floor muscles and lower abdominal in case of lumbar PIVD.
- In case of cervical PIVD activation of cervical core and relaxation of superficial muscles like sternocleido mastoid and sceleni.
- Improve breathing pattern without using neck muscles.
- Neural mobilisation to improve nerve mobility.
- Gradual return to activity.
Physiotherapy management would include :

GOLFERS ELBOW
- Golfers elbow accounts for 0.4% of the population. It usually occurs between the age group of 40- 60, and is much less common than tennis elbow. Women and men are equally affected.
INCIDENCE
ABOUT THE CONDITION
Golfers elbow also known as medial epicondylgia is an overuse injury causing pain on the inside of the elbow joint.
- Training errors which includes
- Improper technique, equipment,
-
Functional risk factors includes lack of strength, endurance, or flexibility.
Occupation-related risk factors includes heavy physical work, excessive repetition, smoking, the presence of comorbidities, and high psychosocial work demands. - Aching pain on the inner side (medial) of the elbow
- Sometimes radiating pain from the epicondyle down into the forearm and wrist
- Often insidious in nature
- Pain increases with forearm motion, gripping, or throwing.
- In athletes, this includes overhead throwing, forearm tennis stroke, or golf swing.
- Pain resolves with rest or discontinuation of activity.
- Elbow stiffness, weakness, numbness, or tingling most common in an ulnar nerve distribution.
- More chronic presentations may report weakness with grip strength.
Risk factors in athletes includes
- This is mostly managed non-surgically.
-
Initially cessation of aggravating activities or decreasing their volume, frequency, or intensity is advised.
- Icing to reduce inflammation and pain in and around the joint during acute stage and post activity.
- Tightness in the extensor muscles causes an overload on the flexors while moving the wrist. So release of the extensor muscles using dry needling or myofascial release helps to reduce pain while movement.
TREATMENT
- Isometric exercises provide analgesic effect for around 40 minutes post exercises. Later concentric and eccentric exercises can be added.
- If conservative management of 6 months fails, steroid injections are given.
PCL INJURY OF KNEE
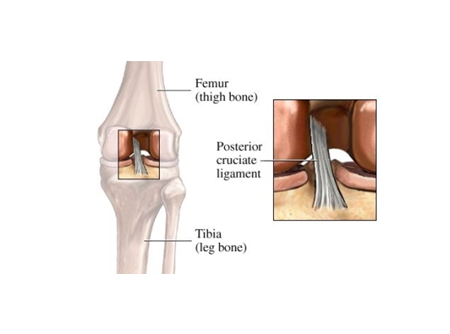
Posterior Cruciate Ligament (PCL) is a ligament within the knee joint. It is similar to the Anterior Cruciate Ligament (ACL), connecting the thigh bone (femur) to the shin bone (tibia). The PCL keeps the tibia from translating/moving back. An injury to the PCL typically requires a powerful force:
- A direct blow to the front of the knee (such as a bent knee hitting a dashboard in a car crash, or a fall onto a bent knee in sports)
- Pulling or stretching the ligament (such as in a twisting or hyperextension injury)
- Pain in semiflexed position, as with ascending or descending stairs or an incline; starting a run; lifting a load; walking longer distance.
- Retropatellar pain
- Swelling and stiffness in case of chondral damage
- Instability while walking on uneven ground
- Medial joint line pain
- Usually full or functional ROM
Symptoms:
- Grade 1 and 2 PCL injury can be managed conservatively. Immobilize the knee in a range of motion brace locked in extension for 2-3 weeks.
- Severe posterior tibia subluxation and instability grade 3 injuries are managed surgically to restore normal knee mechanics and dynamic knee stability, thus correcting posterior tibial laxity.
- Icing for 20 mins every 2 hours in the acute stage for reduction of swelling and pain.
- During the first few weeks, the goals of treatment should focus on effusion control, knee range of motion within prescribed limits, normalization of gait, and reactivation of the quadriceps musculature.
- Enhance proprioception and strengthen the lower extremities in order to perform light low-impact activities pain free and without effusion.
Treatment:
BAKER’S CYST
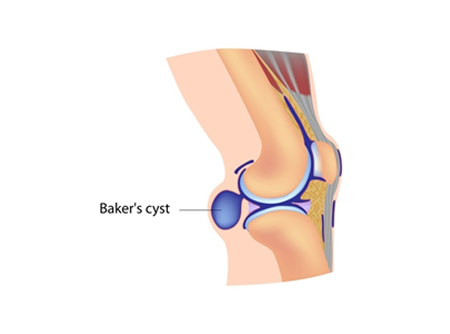
Baker’s Cyst, also known as a popliteal or parameniscal cyst, is a fluid-filled sac that forms in the posterior(behind) aspect of the knee. In adults, Baker's Cysts tend to form in association with degenerative conditions of the knee, for example, secondary degenerative meniscal tears, rheumatoid arthritis, osteoarthritis. In younger generation, it is mostly because of overuse or injury to the knee.
- Sensation of tightness, discomfort, or pain behind the knee.
- Popliteal cysts are located on the medial side of the popliteal fossa just below the crease found at the posterior knee. A palpable swelling at the back of the knee will be firm in full knee extension and soft when the knee is flexed.
Symptoms:
- As a Baker's Cyst enlarges, it may compress surrounding vessels, resulting in lower extremity edema as a result of venous obstruction
- Baker’s Cyst may rupture if, due to rapid accumulation of fluid, pressure within the sac becomes too high. Symptoms may include sharp pain in the knee and calf, swelling or erythema of the calf, and a sensation that feels like water running down the calf.
Other complications:
- Ice pack applied for 20 minutes every two hours or at least 3 to 4times a day to reduce swelling.
- Rest is important. Avoid any activities which aggravate or make the condition worse.
- Kinesio taping helps treat this condition by relaxing and supporting the muscles, reducing pressure in the area of pain, and increasing circulation
- Our Rehabilitation specialists are focused on maintenance of knee flexibility to avoid stiffness that can develop from pain occurring at end range flexion and extension.
- Core Strengthening exercises for the whole leg so that movement in the gait cycle is improved, e.g. unload the knee joint by strengthening quads, hamstrings and glutes, progressively.
- Strengthening exercises for the whole leg so that movement in the gait cycle is improved, e.g. unload the knee joint by strengthening quads, hamstrings and glutes, progressively.
Treatment-
Meniscus
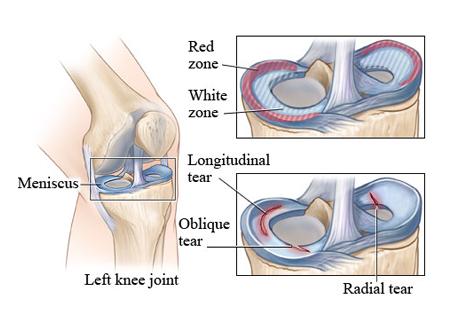
The lateral and medial menisci are crescent-shaped fibrocartilaginous structures that collectively cover approximately 70% of the articular surface of the tibial plateau, and primarily function in load transmission and shock absorption through the tibiofemoral joint. A torn meniscus occurs because of trauma caused by forceful twisting or hyper-flexing of the knee joint. Relatively less force is required to create tears in those with degenerative changes of the menisci, typically seen in adults over the age of 40y, often with concomitant osteoarthritis (OA).
Medial meniscal tears are more common than lateral meniscal tears. Tears that are contained within the outer 1/3 vascular zone of the menisci are "red-red" tears, whereas those with central margins extending into the inner 2/3 avascular zone are "red-white" tears. Tears contained within the inner 2/3 avascular zone are "white-white" tears. Tears located within the red zone have the highest potential for either spontaneous healing with conservative management or successful outcome following meniscal repair.
Epidemiology: Injuries to the menisci are the second most common injury to the knee, with an incidence of 12% to 14% and a prevalence of 61 cases per 100,000 persons. Women are more likely to get meniscus injury than men.
- Pain is commonly intermittent and usually localized to knee joint line
- Sensation of a “pop”, catching or locking
- Swelling is usually delayed, sometimes absent
- Degenerative tears often manifest with recurrent effusions.
- Intermittent inability to fully extend the knee
- Feeling of the knee giving way
- Mechanical block to motion or frank locking can occur with displaced tears.
Symptoms:
- Chronic pain management Physiotherapy includes ice pack application for 20mins every 2 hrs or at least 3 to 4 times a day
- Kinesiology taping for aiding movement or Rigid taping to provide stability at the knee joint and reduce pain and further damage
- Strengthening exercises for the knee: Quadriceps (especially VMO), hamstrings, calves, hip and pelvic muscles in order to take excessive loads off the knee joint and also improve patellofemoral (knee cap) alignment
- Stretching exercises for tight muscles like the glutes, TFL, hip flexors, quadriceps and hamstrings
- Proprioception and balance training to improve your joint position sense and function e.g. walking, running, squatting, hopping and landing, thus minimizing the chances of re-injury.
Treatment:
Prognosis:
Evidence shows that non-operative treatment can be successful especially in the short term and in the presence of osteoarthritis. Partial meniscectomy can preserve some of the function of the meniscus and is beneficial for tears within the avascular white zone. Meniscal repair should be considered for all repairable tears, provided the patient follows-up with the post-surgery rehabilitation approach.
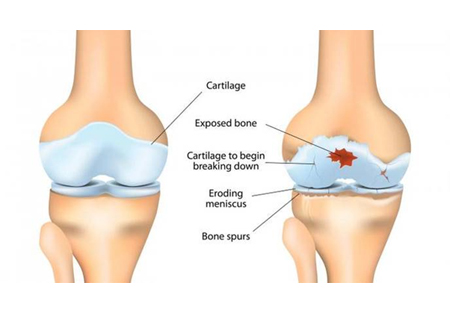
OA: OSTEOARTHRITIS)
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage on the ends of your bones wears down over time. Although osteoarthritis can damage any joint in your body, the disorder most commonly affects joints in your hands, knees, hips and spine. Risk factors for developing OA include age, female gender, obesity, anatomical factors, muscle weakness, and joint injury (occupation/sports activities).
Classically, OA presents with joint pain and loss of function; however, the disease is clinically very variable and can present merely as an asymptomatic incidental finding to a devastating and permanently disabling disorder. The presentation and progression of OA vary greatly from person to person. The triad of symptoms of OA is joint pain, stiffness, and locomotor restriction.
- Muscle weakness and balance issues
- pain hampers activity and resolves with rest
- Swelling
- Joint deformity and instability (patients complain that joint is “giving way” or “buckling,” a sign of muscle weakness).
Patients can also present with:
- Symptoms can usually be effectively managed, although the underlying process cannot be reversed. Staying active, maintaining a healthy weight and other osteoarthritis treatment slows progression of the disease and help improve pain and joint function
- Icing for 20 mins atleast 3-4 times a day, in order to numb the pain and reduce swelling and inflammation around the knee
- Kinesiotaping for support of patella and activation of the muscles around it
- Dry Needling/ Myofascial release to relax the tight Vastus lateralis, internal rotators of hip and knee; as well as to activate the glutes and VMO
- Strengthening exercises of weak and stretching of tight muscles around the knee (Vastus medialis obliquus, Vastus lateralis, hamstring), hip (Iliopsoas, TFL, Gluteus medius and maximus, piriformis) and core (Transverse abdominis)
Treatment:
Prognosis:
There is no cure for osteoarthritis, but the ill-effects of the process can be managed and slowed down by following a good rehabilitation program. The surrounding structures of a joint such as the muscles, tendons and ligaments that can be strengthened, support the joints and take off excessive loads too.
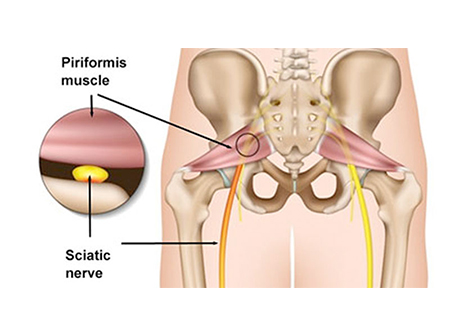
PIRIFORMIS SYNDROME
The sciatic nerve runs just adjacent to the piriformis muscle, which functions as an external rotator of the hip. Hence, whenever the piriformis muscle is irritated or inflamed, it also affects the sciatic nerve, which then results in sciatica-like pain. The sciatic nerve is a thick and long nerve in the body. It passes alongside or goes through the piriformis muscle, goes down the back of the leg, and eventually branches off into smaller nerves that end in the feet.
The diagnosis of piriformis syndrome is not easy and is based on the clinical history and presentation. Other conditions that can also mimic the symptoms of piriformis syndrome include lumbar canal stenosis, disc inflammation, or pelvic causes.
- Trauma to the hip or buttock area
- Piriformis muscle hypertrophy (often seen in athletes during periods of increased weightlifting requirements or pre-season conditioning)
- Sitting for prolonged periods (taxi drivers, office workers, bicycle riders)
-
Anatomic anomalies:
-
Sciatic nerve course/branching variations with respect to the piriformis muscle
- In >80% of the population, the sciatic nerve courses deep to and exits inferiorly to the piriformis muscle belly/tendon.
- Early (proximal) divisions of the sciatic nerve into its tibial and common peroneal components can predispose patients to piriformis syndrome, with these branches passing through and below the piriformis muscle or above and below the muscle
-
Sciatic nerve course/branching variations with respect to the piriformis muscle
Causes of piriformis syndrome include the following:
Symptoms:
Patients with piriformis syndrome will present with the following:
- Chronic pain in the buttock and hip area
- Pain when getting out of bed, climbing stairs
- Inability to sit for a prolonged time
- Pain in the buttocks that is worsened by hip movements
- Symptoms of sciatica: Pain radiating into the back of the thigh, but at times it may also occur in the lower leg at dermatomes L5 or S1
- If pain is caused by sitting or certain activities, try to avoid positions that trigger pain. Rest, ice, and heat may help relieve symptoms.
- Stretching program for muscle length and flexibility.
- Dry Needling or deep tissue release/ foam rolling to reduce muscle tightness around the buttock.
- Deep core stability and hip strengthening exercise to stabilise your hip, pelvis and spine.
Management:
Prognosis:
Short-term symptoms can be reversed within a few days at our chronic pain management clinic. Longstanding symptoms may take a few weeks to address the biomechanical and muscle habits that have predisposed you to the injury.
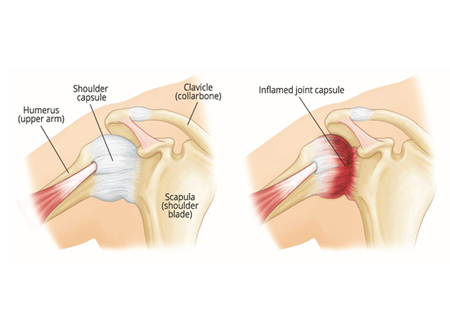
FROZEN SHOULDER
Frozen shoulder/ Adhesive capsulitis (AC), is an insidious painful condition of the shoulder persisting more than 3 months. This inflammatory condition that causes fibrosis of the glenohumeral joint capsule is accompanied by gradually progressive stiffness and significant restriction of range of motion (typically external rotation). However, the patients may develop symptoms suddenly and have a slow recovery phase.
It is characterized by stiffness, pain and limited range of movement in your shoulder due to inflammation and subsequent scarring around the shoulder joint.
Mostly seen in patients with age > 40, peak at the age of 56. Incidence is 2% to 5% of the general population. Female: Male ratio 2:1, In general, bilateral shoulder involvement is rarely simultaneous and instead occurs sequentially.
Patients with Diabetes Mellitus (5 times more likely to develop) 11%, stroke, hyperthyroidism, hypothyroidism, heart diseases, Parkinson’s disease are more prone to developing frozen shoulder.
Frozen shoulder occurs in three phases along with the following symptoms:
1. Acute (painful freezing phase)10-36 weeks
- Pain even at rest
- Stiffness
- Nagging constant pain and worse at night with no response to usual anti-inflammatory and steroids.
- Motions are limited in all directions only in end range.
2. Adhesive stage (frozen) 4-12 months
-Pain gradually subsides but stiffness remains
-Pain only at end ranges of movement.
-Gross reduction of Glenohumeral (arm) movement with near total loss of external rotation.
-Atrophy of deltoid, rotator cuff, biceps, triceps
3. Resolution phase(thawing) 12-42 months
-Spontaneous improvement in ROM
-Minimal pain
-Significant capsular restrictions from adhesions.
- Frozen shoulder therapy includes Taping that provides pain relief, postural cues and assist with promoting proper scapular motion.
- Stretching exercises to increase the core strengthening of the tightened structures. Stretching and release of the inferior glenohumeral capsule and pectoral fascia, insertion of the latissimus dorsi and subscapularis.
- Myofascial trigger point release/ dry needling of the muscles like upper trapezius, levator scapulae, deltoid, infraspinatus, subscapularis which are overworked and causing limitation in shoulder movement.
- mobilization techniques in improving glenohumeral mobility and thereby improving shoulder range of motion.
- Muscles which are prone to weakness in a variety of shoulder dysfunctions include the lower trapezius, serratus anterior, and infraspinatus. So, strengthening of shoulder and scapular muscles to facilitate normal movement patterns.
- In some resistant cases stiffness still persist so surgical intervention might help.
- home program to maintain it.
Treatment-
Prognosis:
The duration of Adhesive capsulitis is from 1 to 3.5 years with a mean of 30 months. In about 15% of patients, the contra-lateral shoulder becomes affected within 5 years.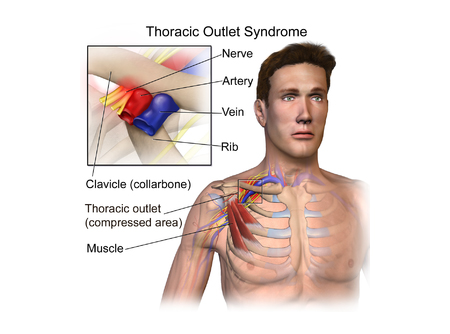
Thoracic outlet syndrome
Thoracic outlet syndrome (TOS) is a group of disorders that occur when blood vessels or nerves in the space between your collarbone and your first rib (thoracic outlet) are compressed. TOS usually occurs in patients who have a cervical rib (extra rib) that directly attaches to C7 vertebra which causes further compression.
TOS affects approximately 8% of the population. It is 3-4 times more frequent in women as compared to men, between the age of 20 and 50 years. Females have less-developed muscles, a greater tendency for drooping shoulders owing to additional breast tissue, a narrowed thoracic outlet and an anatomical lower sternum, these factors change the angle between the scalene muscles and consequently cause a higher prevalence in women.
The mean age of people affected with TOS is 30s-40s; it is rarely seen in children. Almost all cases of TOS (95-98%) affect the brachial plexus; the other 2-5% affecting vascular structures, such as the subclavian artery and vein. This can cause pain in your shoulders and neck and numbness in your fingers.
Thoracic outlet syndrome (TOS) is composed of three types: neurogenic, venous, and arterial.
- Muscle wasting in the fleshy base of your thumb
- Numbness or tingling in your arm or fingers
- Pain or aches in your neck, shoulder or hand
- Weakening grip
Signs and symptoms of neurological thoracic outlet syndrome include:
- Discoloration of your hand (bluish color)
- Arm pain and swelling
- Lack of color (pallor) in one or more of your fingers or your entire hand
- Weak or no pulse in the affected arm
- Cold fingers, hands or arms
- Arm fatigue with activity
- Numbness or tingling in your fingers
- Weakness of arm or neck
- Throbbing lump near your collarbone
Signs and symptoms of vascular thoracic outlet syndrome can include:
- Strengthening exercises of the retractors and rotator cuff of the shoulder namely the rhomboids, trapezius, infraspinatus, teres minor and subscapularis muscles in order to improve posture and keep the thoracic outlet open.
- Stretching exercises for the upper trapezius, levator scapulae, suboccipitals, scaleni, sternocleidomastoid and pectoral muscles.
- These exercises, when practiced over time, may take the pressure off your blood vessels and nerves in the thoracic outlet.
- Myofascial release for the Scaleni and trapezius muscles, as the neurovascular bundle pierces these muscles and continue into the upper limb.
- Gentle neural glides can be done to improve the mobility and pliability of the nerves in the upper limbs.
Treatment-
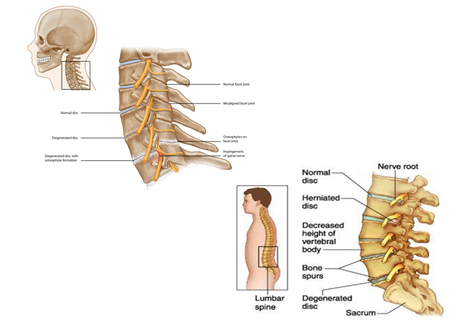
CERVICAL AND LUMBAR SPONDYLOSIS
The term spondylosis is used to define a generalized natural ageing process. Cervical and lumbar spondylosis results from the process of degeneration of the intervertebral discs and facet joints of the cervical and lumbar spine. Biomechanically, the disc and the facets are the connecting structures between the vertebrae for the transmission of external forces. They also facilitate cervical spine mobility.
On radiological finding, 90% of men older than 50 years and 90% of women older than 60 years have evidence of degenerative changes in spine. 70% Of individuals may show bad changes on X- ray but are asymptomatic. Sex ratio reports have been variable but are essentially equal.
- Cervical radiculopathy - Pain most often occurs in the cervical region, the upper limb, shoulder, and/or interscapular region, numbness, heaviness, weakness in upper limb, reduced grip strength
Symptoms:
Cervical spondylosis:
- Neurologic claudication, which includes: lower back pain, leg pain, numbness, heaviness, weakness when standing and walking
Lumbar spondylosis:
- In the acute phase, taping can be done to offload the overused structures
- Spinal mobilization to improve mobility of the spinal segments, thus improving overall mobility
- Dry needling and stretching of paraspinals to relax the tight muscles around neck and back
- After a detailed postural examination, the patient will be taught basic posture correction exercises program to correct the postural deviations caused by muscle weakness or tightness
- Strengthening exercises for the scapula retractors, sub-occipitals, core, transverse abdominis and gluteal muscles, as these muscles provide support and stability to the spine
- In case of any neural symptoms, neural mobilization helps in improving nerve mobility and pliability
- In severe cases, surgery needs to be done after which post-surgery rehabilitation is necessary
Treatment:
MECHANICAL LOW BACK PAIN
Mechanical low back pain refers to back pain that arises intrinsically from the spine, intervertebral discs, or surrounding soft tissues. This includes lumbosacral muscle strain, disk herniation, lumbar spondylosis, spondylolisthesis, spondylolysis, vertebral compression fractures, and acute or chronic traumatic injury.
Low back pain (LBP) is the fifth most common reason for physician visits, which affects nearly 60-80% of people throughout their lifetime. The lifetime prevalence of low back pain is reported to be as high as 84%, and the prevalence of chronic low back pain is about 23%, with 11-12% of the population being disabled by low back pain. In the 2010 Global Burden of Disease study the global age-standardized point prevalence of LBP (from 0 to 100 years of age) was estimated to be 9.4%.
Patients generally present with a history of an inciting event that produced immediate low back pain. The most commonly reported histories include the following:
- Lifting and/or twisting while holding a heavy object (e.g., box, shopping bag,etc. )
- Operating pneumatic tools (e.g., drill machines)
- Sedentary lifestyle which involves Prolonged sitting (e.g., desk job, long-distance truck driving)
- Falls
- Mechanical low back pain is usually cyclic, often referred to the buttocks and thighs
- Morning stiffness or pain is common
- The symptoms are usually worsened by activity and improved partially by rest
- Physical activity, particularly bending, extending, twisting and lifting, commonly aggravates the symptoms, whereas restriction of pain-producing activities results in improvement at least temporarily.
- Pain becomes worse over the course of the day and relieved by the change of position
Typical physical findings are nonspecific, including restricted range of motion of the spine, tight hamstring muscles, paravertebral muscle spasms, muscular trigger points, tenderness and aggravation of symptoms on flexion or extension and straight leg raising tests.
- According to recent advances and research, movement is good for your back
- Corrective exercises for postural deviations, helps strengthen the muscles of and around the spine
- Tight hip and back muscles can impede mobility of the spine, as muscles are connected like a chain in our body, thus stretching exercises help to maintain good mobility not only at the spine, but at all joints as well.
- Dry needling, soft tissue release and taping can be used to relieve pain and provide additional support to the muscles of the back.
- Taking regular breaks at work for those with sedentary jobs and ergonomic changes for e.g. adjustment of chair and desk suitable for one’s body structure, correct techniques of lifting weight, etc. as per the ergonomic guidelines, prove effective in preventing recurrence of pain episodes.
- Basic strength requires 6-8 weeks to build, post which, functional exercises can be taught, based on the type of occupational or sporting demands the individual requires to achieve.
Treatment:
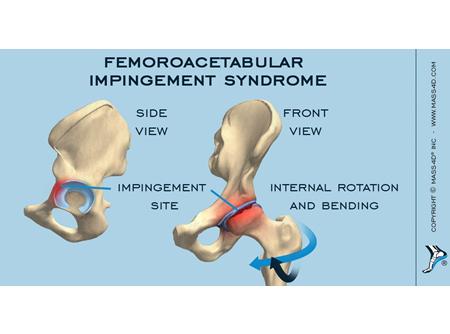
HIP IMPINGEMENT
The incidence of hip impingement in patients with groin pain is 0.44% in the entire population.
Hip impingement in medical terms is known as Femoroacetabular impingement (FAI), is a condition in which the anatomic abnormalities of the femoral head and/or the acetabulum result in an abnormal contact between the two during hip motion, especially in positions of hip flexion and rotation, leading to cartilage and labral damage and hip pain. This results in increased friction during hip movements that may damage the joint.
- Stiffness in the groin or front of the thigh and/or a loss of your hip's full range of motion.
- Many athletes often describe pain in the groin with deep flexion or rotation of the hip during activity
- Occasionally, a popping or clicking in the front of the hip
- Pain may also radiate along the side of the thigh and in the buttocks. It is important to rule out other causes of pain in this area which may originate in the low back or abdomen
- As the condition progresses, pain with more subtle activities, such as sitting for a long time or walking up a hill
- Night pain or when walking on flat ground suggests that the cartilage cushioning the ball and socket has begun to break down and wear away, a condition known as Osteoarthritis (OA)
Symptoms:
- Patient education to avoid pivoting motions, especially under load, since the acetabulum rotates on a loaded femur, thus increasing force across the labrum.
- Advising modification of functional activities and counselling on joint protection strategies and avoidance of symptom-provoking activities to prevent further damage
- Manual therapy such as hip joint mobilization for capsular restrictions while avoiding end-range flexion and internal rotation
- Exercises and activities including stretching of tight hip muscles and strengthening of core, hip, and leg muscles (based on any observed asymmetry in rotation), in order to improve range of motion at the hip joint and strength
- Neuromuscular re-education that focuses on multi-joint patterns to improve movement coordination
- In case of a sportsman, then progression to sports physiotherapy training involving agility and speed training is important for return to play
- When a major damage is involved, surgical intervention needs to be done and post-surgical rehabilitation is necessary.
Treatment

Iliotibial band friction syndrome
Iliotibial band friction syndrome (ITBFS) is the most common injury of the lateral side of the knee in runners, with an incidence estimated to be between 5% and 14%. It has even been reported that ITFBS is responsible for 22% of all lower extremity injuries in general.
Iliotibial band syndrome (ITBS or IT band syndrome) is an overuse injury of the connective tissues that are located on the lateral or outer part of thigh and knee. It causes pain and tenderness in those areas, especially just above the knee joint. Iliotibial band syndrome is the most common cause of lateral knee pain in runners and bicyclists.
Weak hip, adductors and calf muscles, play a larger role in the development of ITB syndrome. If the symptoms are ignored, the inflammation can continue and scarring develops in the bursa, decreasing knee range of motion and causing increasing pain with decreasing activity.
- Pain on the lateral side of the knee is the most common symptom of iliotibial band syndrome and is due to inflammation of the area where the band crosses back and forth at the femoral epicondyle
- A sensation of stinging or needle-like pricks that are often ignored. This can gradually progress to pain every time the heel strikes the ground and finally can become disabling with pain when walking or when climbing up or down steps
- Snapping or popping sound at the knee, and there may be some swelling either where the band crosses the femoral epicondyle or below the knee where it attaches to the tibia
- Occasionally, the pain may radiate along the course of the IT band all the way up to the outer side of the thigh to the hip.
Symptoms:
- Evaluation of the underlying cause of the problem and assessing muscle strength and balance and/or flexibility and gait analysis (watching a person walk, run, or cycle), is the first step
- Shoe orthotics may be useful if there is a gait problem, pelvic tilt, or leg-length discrepancy as a potential cause of IT band syndrome.
- Stretching exercises, foam rolling, soft tissue release, Dry needling of Vastus lateralis, hamstring, tibialis anterior and calf muscles to increase flexibility of IT band and related structures.
- Strengthening of the hip abductor and gluteal muscles is of utmost importance as these group of muscles provide stability and take the excessive loads off the IT band and knee.
- The main goal is to work with combinations of running, jumping, agility and balance exercises, with a clear emphasis on using the proper technique taught by our rehabilitation specialist’s.
Treatment:

Hamstring strain
The hamstrings are the three muscles at the back of the thigh. At the top they are attached to the 'sit bone' of the pelvis. The lower ends cross the back of the knee joint and are then attached to the bones of the lower leg:
- Semitendinosus - attaches to the back of the shin bone (tibia) on the inside of the back of the knee
- Semimembranosus - also attaches to the back of the shin bone (tibia) on the inside of the back of the knee
- Biceps femoris - attaches to the top of the smaller bone of the lower leg (fibula) on the outside of the back of the knee.
Hamstring strain injuries remain a challenge for both athletes and clinicians, given the high incidence rate, slow healing, and persistent symptoms. Prevalence ranges from 8 to 25 percent, depending upon the sport. In soccer it is the most frequent injury.
Hamstring strains are common in sports with a dynamic character like sprinting, jumping, where quick eccentric contractions are regular. Besides running, kicking is another activity in which hamstring muscle strain injuries occur frequently.
Hamstring strains are caused by a rapid extensive contraction or a violent stretch of the hamstring muscle group which causes a high mechanical stress. This results in varying degrees of rupture within the fibres of the musculotendinous unit.
Acute or sudden hamstring strains usually happen in two ways, either sprinting related or stretch related. During sprinting the hamstring muscles work extremely hard to decelerate the shin bone just before the foot strikes the ground and it is at this point that the hamstring is most likely to tear. Stretch related injuries usually occur higher at the back of the thigh in the tendon of the semimembranosus muscle. Sprinting related hamstring injuries often feel worse but recover more quickly, whereas stretch related hamstring strains can take longer to heal as the injury is more likely to the tendon where blood flow is lower.
Symptoms of a hamstring strain include:
-
Hamstring strains are graded:
-
Grade 1:
- Overstretching without tearing of muscle or tendon fibres
- Symptoms may not present until activity is over
- Usually no loss of muscular strength or flexibility
- Increased tightness in the muscle during stretch or through a full range of motion
- A feeling of pain may be reported with sitting or while walking uphill or ascending stairs
- Depending on the severity, weight bearing activities may or may not be possible, walking properly may be possible and there will be minimal swelling
-
Grade 2:
- Partial tear in the muscle
- Muscular strength and flexibility in reduced
- Pain is more immediate and more severe than the pain of a Grade 1 strain
- Pain on stretch and contraction of the muscle, and is usually sore to touch
- Limping is likely during walking and occasional sudden twinges of pain during activity may occur
- Bending the knee against resistance will cause pain and there may be some difficulty in fully straightening the knee.
-
Grade 3:
- Severe or complete rupture of the muscle
- Sudden, sharp pain in the back of the thigh
- Walking is not possible without pain
- After a few days with Grade 2 and 3 injuries, a large bruise may appear below the injury site caused by bleeding within the tissues
- May require surgical repair
-
Grade 1:
- The immediate treatment of any soft tissue injury consists of the RICER protocol – rest, ice, compression, elevation and referral. RICE protocol should be followed for 48–72 hours. The aim is to reduce the bleeding and damage in the muscle. The muscle should be rested in an elevated position with an ice pack applied for 20 minutes every two hours
- After the initial acute stage very gentle stretching exercises for the hamstring can begin
- Tendons like loads, but not erratic loads. Progressive loading of tendons has to be done in order to strengthen the hamstring muscles and avoid recurrence of injury
- Strengthening exercises for Glutes and core are an important component of the rehab program in order to equally manage the excessive load placed on the hamstring muscle
- Eventually sport specific exercises and drills should be performed before returning to full competition or training.
- Gradually the athlete progresses to gentle jogging and shuttle runs. Finally, acceleration runs and sprinting speed is gradually developed.
Treatment-
Prognosis:
Timeframes for rehabilitation and return to sport vary depending on the nature and severity of the strain. As a general rule, Grade 1 hamstring strains should be rested from sporting activity for about three weeks and Grade 2 injuries for a minimum of four to eight weeks. In the case of a complete rupture (Grade 3 strain), the muscle may have to be repaired surgically and the rehabilitation to follow will take about three months.
Premature return to sport and inadequate rehabilitation will reduce the impact of sport injury rehabilitation program and increase the chances of re-injury. Full stretch and strength should be achieved in addition to the ability to perform full speed training. Assessment of sport-related activities, such as twisting, jumping and changing direction suddenly should also be evaluated.
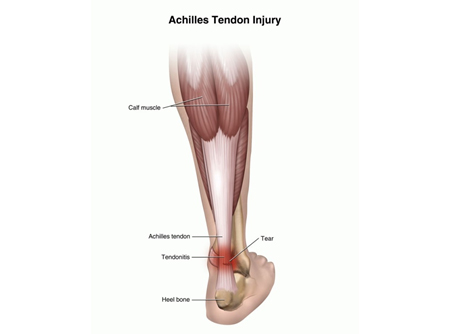
Achilles Tendinopathy/ Tear
The gastrocnemius/calf muscle consists of 2 heads. The medial head originates from the posterior medial femoral condyle while the lateral head arises from the posterior lateral femoral condyle. The gastrocnemius muscle is vulnerable to injury because it crosses 3 joints: knee, ankle and subtalar joint.
Tendo Achilles injury is common in young athletes involved in high impact plyometric sports such as racquet sports, running, basketball, football, and skiing. Calf injuries occur more commonly in men than in women,In the older age group tears usually occur in the fourth to sixth decade of life due to degeneration.
Symptoms:
Grade 1 Injury (Mild)
:
The patients may feel a sharp pain at the time of injury or pain with activity. They are usually able to continue the activity. There may be no or minimal loss of strength and range of motion. MRI study exposes bright signals on fluid-sensitive sequences with less than 5% feathery appearance of muscle fiber involved. Grade 1 injury indicates less than 10% of muscle fibers disrupted.
Grade 2 Injury (Moderate)
The patient cannot walk at the moment of injury. The patient may complain of weakness during ankle dorsiflexion and plantar flexion. Change in the myotendinous junction due to edema or hemorrhage. Grade 2 injury implies 10% to 50% disruption of muscle fibres.
Grade 3 Injury (Severe)
There may be a palpable defect on the affected calf. The MRI findings include complete disruption of continuity of muscle, wavy tendon morphology and retraction and extensive hemorrhage or edema. Grade 3 injury indicates 50% to 100% disruption of muscle fibres
- Initially gentle stretching of the calf given along with soft tissue release and foam rolling
- Tendons like loads, but not erratic loads. Hence, progressive loading exercises are most effective for the core strengthening of the calf muscle. This also prevents recurrence of the injury
- Icing of the calf muscle for 20mins every 2 hours can help curb the acute inflammatory effects of the strain
Treatment- depending upon the grade of injury treatment differs.
Prognosis:
Most studies indicate that gastrocnemius strains mostly have a good prognosis. Most patients can have a marked decrease in pain and return to exercise after adequate management.